E is for Exit
- Thoracic aortic root
-
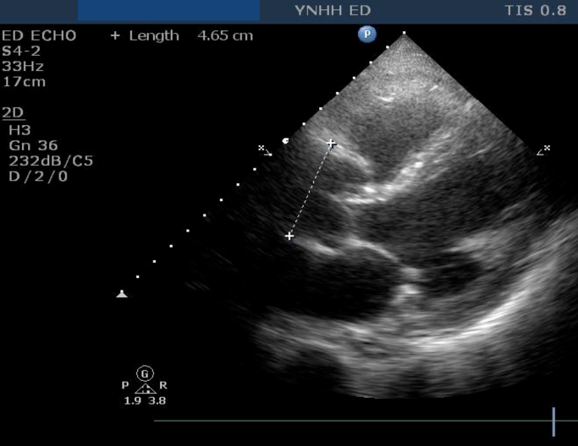
Best seen on parasternal long axis
- Not all aneurysms dissect
- Not all dissections are aneurysmal
- But there is a strong association
- Measure outside wall to inside wall (leading edge method)
-
At sinuses of Valsalva, or widest part
- Normal <4.0cm
- Borderline 4.0-4.5cm
- Aneurysmal >4.5cm
Narration
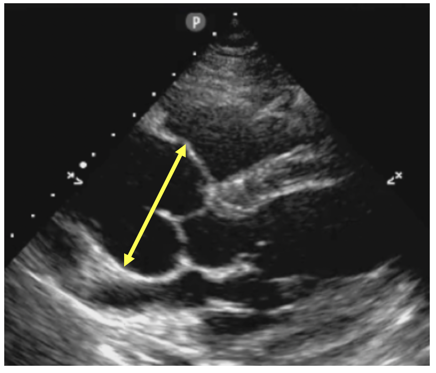
So the fourth of our five E's is the exit, and that is really the thoracic aortic root as it exits the left ventricle. This is best seen on a parasternal long axis and the reason we look at it is because it can be a clue for possible thoracic aortic dissection or aneurysm. It is important to understand that not all aneurysms dissect, and not all dissections are aneurysmal, but there is a strong association. So, when you see somebody with symptoms like chest pain, syncope, shortness of breath and they have a dilated thoracic aortic root you should consider the possibility of an aortic aneurysm or a dissection going on that could be causing symptoms. In order to measure this we go from the outside wall to the inside wall, which is called the leading edge method, it is the first edge that the ultrasound beam hits going from proximal to distal, and ideally we measure it at the sinuses of Valsalva, the little outpouchings right at the beginning of the aortic root, and that's often the widest part. Although, you have to keep your eyes open sometimes it gets wider after, we'll show some examples of this, and really you want to measure the aorta at the widest part. We consider normal under 4 cm, borderline about 4-4.5 cm, sometimes these will still be normal on CT if you do them, but when you measure it on echo and it is over 4.5 cm it is definitely abnormal.
Thoracic aortic diameter in dissection
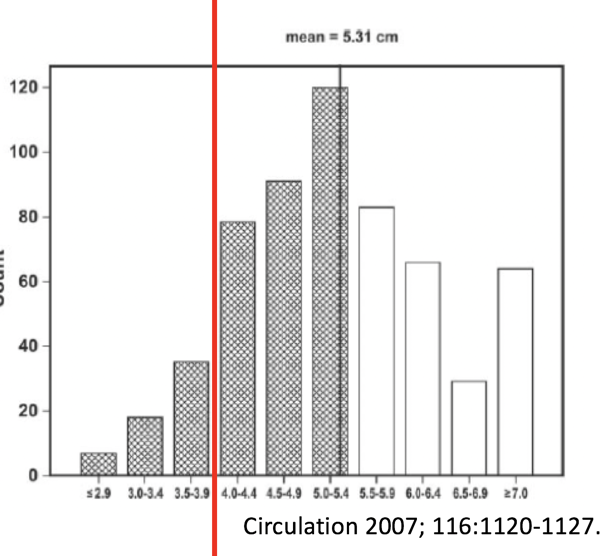
 Acad Emerg Med 2012; 19:244–247
Acad Emerg Med 2012; 19:244–247

Narration
We were among the first in the country to show that emergency physicians could accurately measure the thoracic aortic root and that it would correspond to aneurysmal disease as seen on CT, and again we just want to say that not all aneurysms dissect and not all dissections are aneurysmal, but there is a strong association and this paper from Circulation in 2007 shows dissecting aneurysms and the width of the thoracic aorta and you'll notice that nearly all of them had a dilation that was 4 cm or greater. The aneurysms will actually expand when they start to dissect, so you get a wider thoracic aortic root and you can really pick up these sometimes sooner than otherwise using point of care ultrasound or point of care echo.

Narration
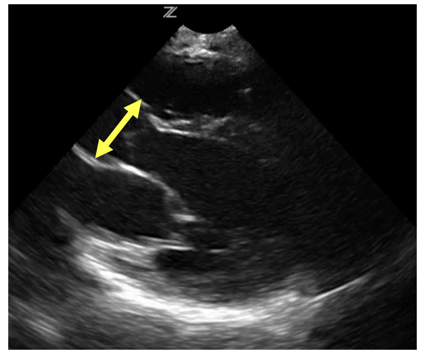
So this is a classically dilated thoracic aorta seen at the sinuses of Valsalva, those little out-pouchings right beyond the aortic valve. If you were to measure this it would probably be 4.5-5 cm. This is a simple dilated thoracic aortic root that may be associated with dissection, we don't see a flap, but it is a clue that there is pathology in the aorta.
PSLA
Slight dilation at sinuses of Valsalva then much larger
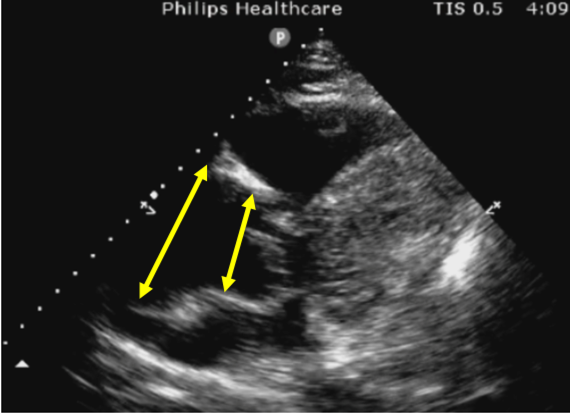

Narration
So here is an example of what we were talking about, where the initial part of the aorta is somewhat dilated, but then as it goes a little bit further along, we can see that the thoracic aortic root really expands further, and this is an aneurysm that is a little bit further along than the sinuses of Valsalva. So if you see an area of aorta that is bigger, then measure the largest part that you can, trying to do it from the outside wall to the inside wall.
Occasionally actual dissection flap can be seen
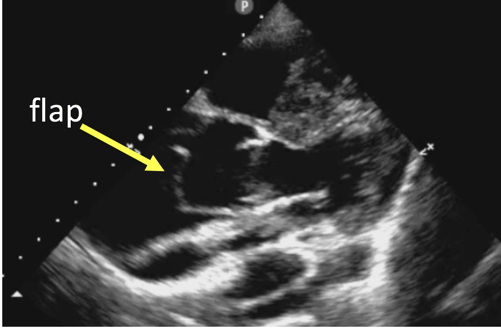

Narration
Occasionally you'll see something like this, where we have a dilated thoracic root and within that you can actually see the flap, which is the dissection of the walls of the aorta - you can see the true lumen and the false lumen flapping back and forth each time the aortic valve opens. Again, it's unusual to really see a flap this clearly and the presence of thoracic aortic dilation with chest pain or other symptoms should clue you in that there may be a flap and you're just not seeing it. But this an extreme example of a vigorously moving aortic dissection flap on the parasternal long axis view.

Narration
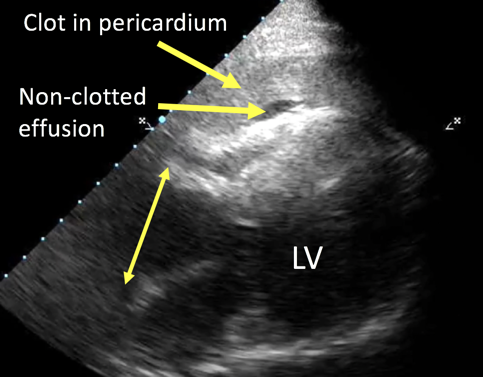
So here the E is for both exit and effusion. This was actually the case that we talked about at the beginning of this lecture, the guy who came in and passed out after going through the metal detector, and as we start to look at this, again it’s a little fuzzy and real world, but you can see there is dilation of the thoracic aortic root, as shown in the diagram on the lower left, and then there is both a small non clotted effusion or black area around the heart with a fairly large homogenous gray clot throughout the pericardium. The combination of a dilated thoracic root and a pericardial effusion is essentially type A dissection until proved otherwise. This is somebody you want CT surgery involved in sooner rather than later. Certainly, if they're stable you can get them to CT or CTA as soon as possible, but that combination can be deadly and needs to be acted on quickly.
?
main Pv# 1 , InitialPages , pix False , #Drops 0 ;
trys 0