Other Procedures
Other Procedures
Narration
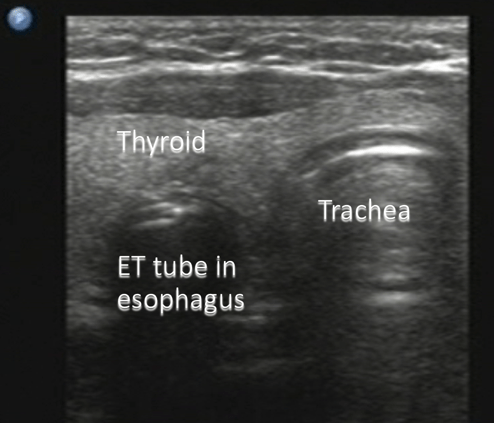
So most commonly we are going to use ultrasound to guide procedures where we are putting a needle into a fluid filled space such as a vessel, or a joint effusion, or something like that, but we can also it for other procedures. This is an example of an intubation. We are looking at the neck using a linear probe seeing the thyroid tissue and the trachea and in this case you can see the endotracheal tube going in lateral to the trachea in the esophagus. This is a not well-placed esophageal intubation you can see by ultrasound that we then removed the tube.
Other Procedures
Narration
Here is a diagram showing the two structures: the trachea to the right of the screen, the thyroid tissue is very homogenous. If you look at that movie you can see the endotracheal tube entering the esophagus again lateral to the trachea. This could be an adjunct to procedural intubation.
Peritonsillar Abscess
Randomized trial showed improved success with US guidance
Constantinto et al., “Randomized trial comparing intraoral ultrasound to landmark-based needle aspiration in patients with suspected peritonsillar abscess”, Acad Emerg Med 2012; 19: 626-631.
Narration
Here is another example of a procedure that is somewhat uncommon, could be considered looking at fluid, but this is using what we call the endocavitary probe, be careful not to call it the endovaginal probe because we are putting it in the mouth in this case to visualize a peritonsillar abscess. In this case, you can see a complex structure that is fluid filled with some septations and in the far field you can see the vasculature including the carotid artery that you obviously don't want to put a needle in. There has been a randomized trial that shows that using ultrasound guidance for peritonsillar abscess will improve your success. It can tough to do dynamically, but I will often use this to determine where the abscess is, if there actually is an abscess, and how deep it is, and make sure I'm not going to inadvertently puncture the carotid.