Thoracentesis & Paracentesis
Thoracentesis
- Ultrasound quantifies better than CXR
- Can identify complex/ loculated effusions
- Can estimate volume
- May substantially reduce incidence of pneumothorax
- Static technique acceptable

Narration
So thoracentesis and paracentesis are two procedures where you are typically accessing a fairly large volume of fluid in a particular body cavity. In this case, a static technique may be appropriate, where you find the area where the pocket of fluid is closest to the skin, you mark it using indentation or a skin marking pen, put down the probe, make it sterile, and then access that fluid filled volume. So for thoracentesis, ultrasound has some particular advantages. It can quantify fluid certainly better than chest x-ray and often better than CT scan. It can also identify complex or loculated effusions that are difficult to tap, it can estimate the volume, and there is evidence to show that using it appropriately will decrease the incidence of pneumothorax. So when you are doing this you may again find the pocket of fluid, identify the diaphragm.
Thoracentesis
- Ultrasound quantifies better than CXR
- Can identify complex/ loculated effusions
- Can estimate volume
- May substantially reduce incidence of pneumothorax
- Static technique acceptable
Narration
You can do a dynamic approach, as shown here, we see that needle coming in, it’s getting a little close to the diaphragm, but not quite there; but often times I'll do this using a static technique where the ultrasound probe is down and I just know which direction to go in.
Paracentesis
Narration
Paracentesis is another one where you can use ultrasound first of all to make sure there is fluid you can tap. The New England Journal has noted that bedside ultrasonograpy is ideal to find this pocket of fluid and to access it particularly in patients who have scarring or other problems.
Paracentesis
Avoid inferior epigastric vessels
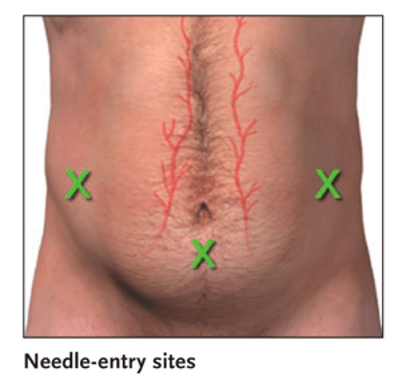
Narration
When you do a paracentesis, one of the main things you want to avoid are the inferior epigastric vessels and you can do this using the landmark technique and picking the right place to go, or you can use ultrasound to visualize those epigastric vessels. here we see color flow showing the artery and the paired veins right at the border of the peritoneum and ideally you would avoid this with a needle.